Quality Sleep with GreenKey4Life Powered by SleepScore APIs
Actionable insights and well-defined guidance are now at your fingertips with GreenKeyforlife .
Using SleepScore APIs, GreenKeyforlife provides a solution to the pressing need of sleep deprivation, enhancing engagement and driving better health outcomes. This is achieved through highly personalized sleep journeys and coaching, all based on the latest behavioral and circadian science, and supported by extensive studies and data.

Since SleepScore APIs are leading the way with the world’s first and only reimbursed sleep improvement program, GreenKey Health feels immensely proud to incorporate SleepScore APIs for better and improved sleep health for our users.

GreenKey4Life: Driving Growth with SleepScore APIs
With GreenKey4Life , we just don’t enhance sleep outcomes but rather boost engagement, improve retention, and optimize health and wellness results. By leveraging user sleep data such as chronotype, behaviors, and motivations, we deliver better outcomes.

Consistent Engagement
3-4x
daily
Increased Retention
60-90%
after 30 days
More Exercise
up to 48%
increase in fitness activity
More Sleep
10-26
more hours of sleep per month*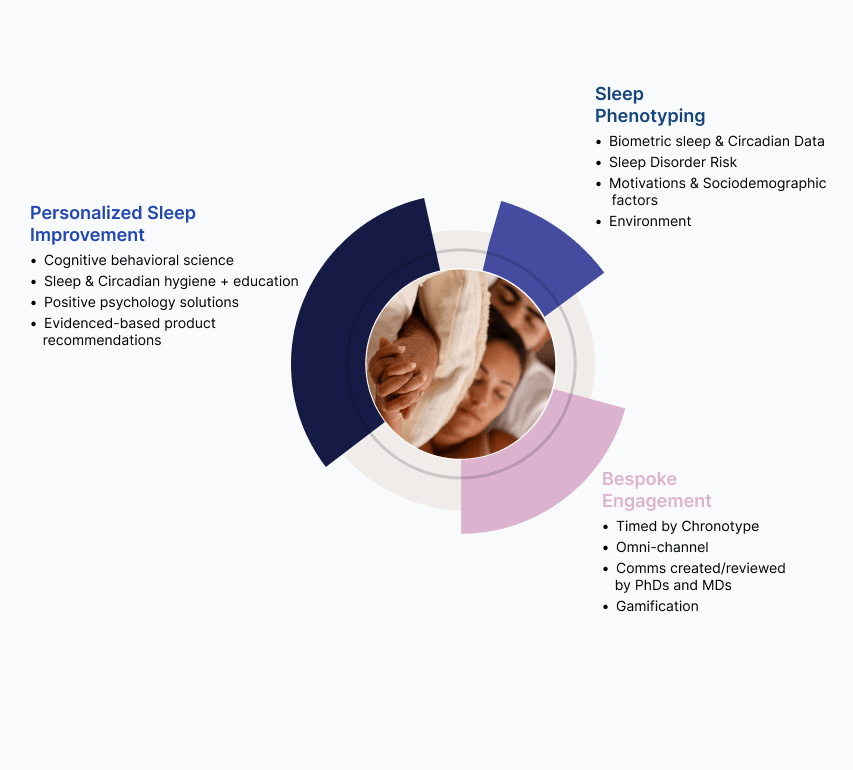
GreenKey4Life Understands Consumers’ Unique Sleep Needs
We understand our users’ requirements and how sleep deprivation may affect them and their everyday life. Therefore, we leverage robust data collection, analysis, and precise API delivery through SleepScore API integration. GreenKey4Life is designed meticulously to empower the users to confidently take charge of their sleep journey through actionable habits, ongoing learning, continuous improvement, and adaptive guidance.
GreenKey4Life x SleepScore APIs
Leading the Way in Sleep Innovation
Sleep Data APIs
Effortlessly collect sleep data measured through wearables and apps.
Sleep Content APIs
Access thousands of engaging sleep and well-being related content materials for better guidance and support.
Authentication APIs
Ensure secure connections across diverse systems and platforms to collect, analyze, and track progress, seeking optimal sleep health.
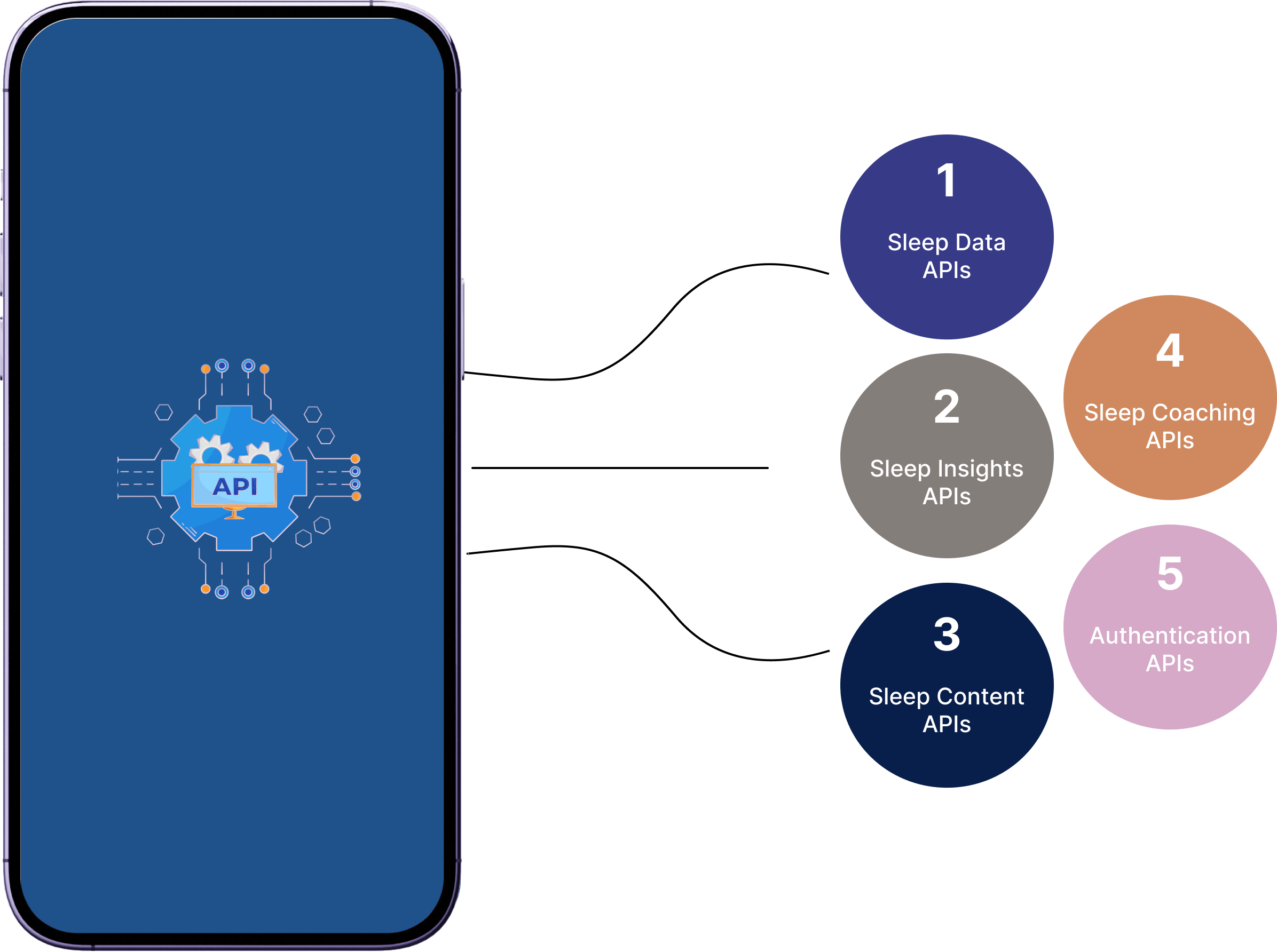
Sleep Insights APIs
Deliver actionable sleep insights tailored to individual requirements, activities, and preferences.
Sleep Coaching APIs
Provide personalized and adaptive sleep coaching rooted in science and Cognitive Behavioral Therapy (CBT) for optimal sleep throughout the night.
Why is Sleep Important? The Unrecognized
Hero Behind Health & Wellness
Weight Management / Loss:
- 55% less fat loss
- 66% more lean body mass loss
- 15% impaired hormone regulation (Ghrelin, Leptin)
Women's Health
- 2x higher risk of menstrual irregularity
- 3.8x higher risk of miscarriage 10
- 20% reduced fertility
Mental health
- 2.5x higher risk of frequent mental distress
- 75% with mental health issues and depression affected
Longevity
- 26% higher risk of mortalityle
- 20-34% higher risk of heart attack
- 30% higher risk of dementia
- 40% higher neurodegeneration
- 40% lower glucose metabolism
Fitness / Athletics
- 30% less time to exhaustion
- 2x higher risk of injury
- 9% lower accuracy?
- 8% longer reaction time
Skin Care / Appearance
- 18% lower hydration?
- 17% lower blood flow
- 5% lower elasticity
- 4% lower translucency
- 2.9% lower desquamation
Why SleepScore?
Backed by Science and Data Experts
Trusted by Various Industries
Device and Data Compatible
Offers Seamless Sync
Professional Customer Service
Supported by ResMed
References:
- Nedeltcheva, A. V., Kilkus, J. M., Imperial, J., Schoeller, D. A., & Penev, P. D. (2010). Insufficient sleep undermines dietary efforts to reduce adiposity. Annals of internal medicine, 153(7), 435-441.
- Taheri, S., Lin, L., Austin, D., Young, T., & Mignot, E. (2004). Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS medicine, 1(3).
- Blackwelder, A., Hoskins, M., & Huber, L. (2021). Effect of Inadequate Sleep on Frequent Mental Distress. In Preventing Chronic Disease (Vol. 18). Centers for Disease Control and Prevention (CDC).
- Nutt, D., Wilson, S., & Paterson, L. (2008). Sleep disorders as core symptoms of depression. Dialogues in clinical neuroscience, 10(3), 329-336.
- Azboy, O., & Kaygisiz, Z. (2009). Effects of sleep deprivation on cardiorespiratory functions of the runners and volleyball players during rest and exercise. Acta Physiologica Hungarica, 96(1), 29-36.
- von Rosen, P., Frohm, A., Kottorp, A., Fridén, C., & Heijne, A. (2017). Multiple factors explain injury risk in adolescent elite athletes: applying a biopsychosocial perspective. Scandinavian journal of medicine & science in sports, 27(12), 2059-2069.
- Mah CD, Mah KE, Kezirian EJ, Dement WC. The effects of sleep extension on the athletic performance of collegiate basketball players. Sleep. 2011 Jul 1;34(7):943-50
- Latiri, I., & Dogui, M. (2016). Effects of one-night sleep deprivation on selective attention and isometric force in adolescent karate athletes. The Journal of Sports Medicine and Physical Fitness, 57(6), 752-759.
- Nam, G. E., Han, K., & Lee, G. (2017). Association between sleep duration and menstrual cycle irregularity in Korean female adolescents. Sleep medicine, 35, 62-66.
- Samaraweera, Y., & Abeysena, C. (2010). Maternal sleep deprivation, sedentary lifestyle and cooking smoke: Risk factors for miscarriage: A case control study. Australian and New Zealand Journal of Obstetrics and Gynaecology, 50(4), 352-357.
- Ahlborg Jr, G., AXELSSON, G., & Bodin, L. (1996). Shift work, nitrous oxide exposure and subfertility among Swedish midwives. International journal of epidemiology, 25(4), 783-790.
- Hublin, C., Partinen, M., Koskenvuo, M., & Kaprio, J. (2007). Sleep and mortality: a population-based 22-year follow-up study. Sleep, 30(10), 1245-1253.
- Daghlas, I., Dashti, H. S., Lane, J., Aragam, K. G., Rutter, M. K., Saxena, R., & Vetter, C. (2019). Sleep duration and myocardial infarction. Journal of the American College of Cardiology, 74(10), 1304-1314.
- Sabia, S., Fayosse, A., Dumurgier, J., van Hees, V. T., Paquet, C., Sommerlad, A., … & Singh-Manoux, A. (2021). Association of sleep duration in middle and old age with incidence of dementia. Nature Communications, 12(1), 2289.
- Gottlieb, E., Egorova, N., Khlif, M. S., Khan, W., Werden, E., Pase, M. P., … & Brodtmann, A. (2020). Regional neurodegeneration correlates with sleep-wake dysfunction after stroke. Sleep, 43(9).
- Spiegel, K., Tasali, E., Leproult, R., & Van Cauter, E. (2009). Effects of poor and short sleep on glucose metabolism and obesity risk. Nature Reviews Endocrinology, 5(5), 253-261.
- Kim, M. A., Kim, E. J., Kang, B. BY., & Lee, H. K. (2017). The effects of sleep deprivation on the biophysical properties of facial skin. Journal of Cosmetics, Dermatological Sciences and Applications, 7(1), 34-47.
What patients are saying about Zzoma
Take a closer look at positional OSA
Defining positional OSA
- It empowers its users to seamlessly monitor and measure sleep, providing sleep insights.
- It offers a full range of sleep health products and services.
- Accelerates monitoring, analysis, and potential treatment solutions.