Comparison of Zzoma Positional Sleep Therapy in Patients with OSA
Obstructive Sleep Apnea (OSA) Syndrome is highly prevalent, affecting 2% of women and 4% of men in the general population. Recent studies have identified OSA as an independent risk factor for a number of cardiovascular diseases, including hypertension, stroke, congestive heart failure and coronary artery disease. CPAP is the most common treatment for patients with OSA, as it has been shown to be efficacious. However, compliance with CPAP therapy is poor, with studies demonstrating compliance rates of less than 50%. The treatment is often uncomfortable and burdensome to the patient, with reported intolerance to the pressure, nasal congestion, claustrophobia or discomfort related to the mask. Other therapeutic options include surgical intervention of the upper airway, weight loss, the use of an oral appliance, and when indicated, positional therapy.
Recent data has identified that positional obstructive sleep apnea, where patients have the majority of their sleep-disordered breathing events when lying supine, is quite prevalent in patients with mild and moderate OSA. Using the definitions of the American Academy of Sleep Medicine (AASM), Mador et al found that 50% of patients with mild OSA (apnea-hypopnea index [AHI] of 5-15 events/hr) and 19% of patients with moderate OSA (AHI of 15-30 events/hr) have positional OSA. Again, using the AASM definition of normal as being < 5 events/hr, these patients when in the non-supine position would decrease their AHI to < 5 events/hr.
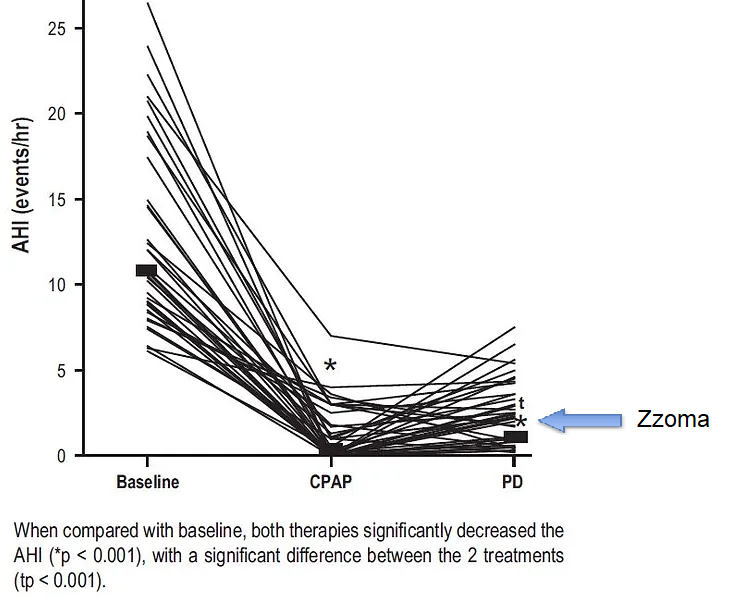
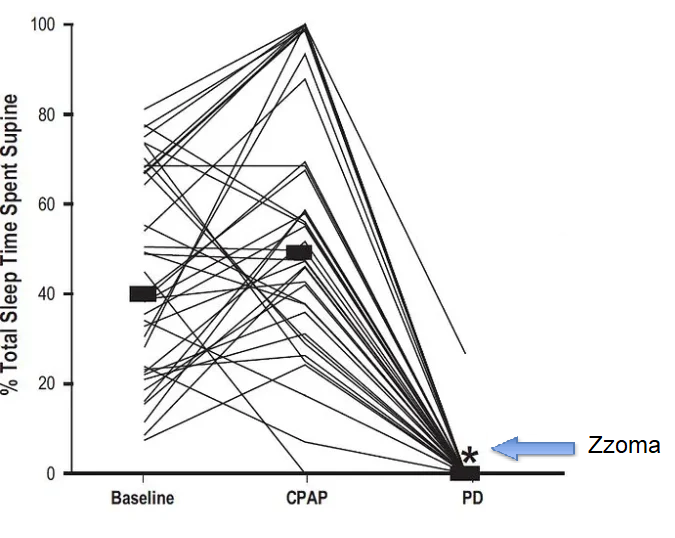
As a result, we evaluated the effects of a new positional device (Zzoma Positional Device) in patients with positional OSA and compared it to conventional CPAP therapy, specifically utilizing definitions of success as a normalization of the AHI to < 5 events/hr. The Zzoma Positional Device has been designed along the “ball in the backpack” concept that has been used in previous studies. However, the shape and the design of the Zzoma Positional Device has been improved over this simplistic concept in order to maximize effectiveness and comfort in keeping the patient sleeping in the lateral position.
- In patients with positional OSA, Zzoma is equivalent to CPAP therapy at normalizing the AHI to less than 5 events per hour in addition to decreasing the AHI by over 50.
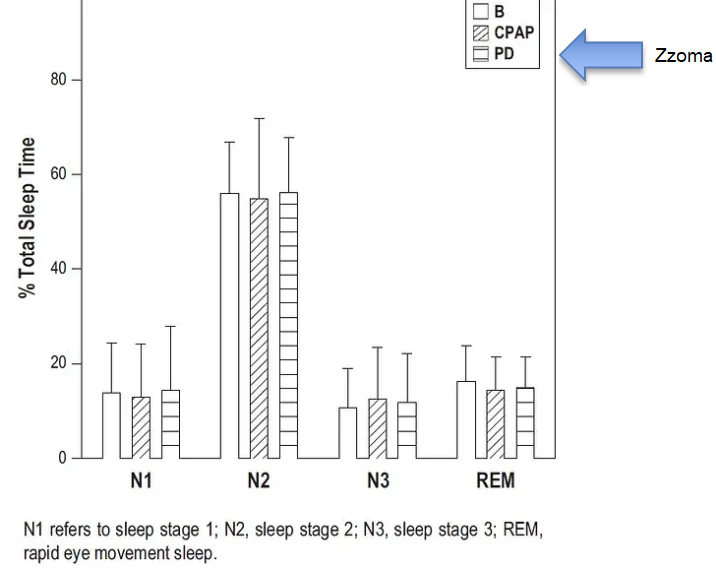
- Zzoma is similar to CPAP therapy in regard to its effects on sleep quality and nocturnal oxygenation
- There is minimal night-to-night variability in the non-supine AHI in patients with positional OSA.
- Zzoma is effective at maintaining patients in the non-supine position throughout the night.
There Were 4 Major Findings in This Study
For More Studies Look At
Use of a diagnosis-treatment algorithm for OSA that incorporates positional therapy demonstrates that positional OSA is prevalent and that positional therapy can often be prescribed as an appropriate first-line therapy and at a lower cost as compared to CPAP therapy. Read more…
Incorporating positional therapy into the treatment algorithm for OSA is cost effective. Study Objectives: The primary aim of this study was to determine cost effectiveness of positional therapy in a treatment algorithm. The new study was conducted out of Temple University in Philadelphia and included patients from the Law Enforcement Health Benefits (LEHB) organization. Read more…
American College of CHEST: Physicians Prevalence of Positional Sleep Apnea in Patients Undergoing Polysomnography. Study Objectives: The primary aim of this study was to determine the prevalence of positional obstructive sleep apnea using a functional definition. Positional sleep apnea was defined as a total apnea-hypopnea index (AHI) >4 with a > 50% reduction in the AHI between the supine and non supine postures and an AHI that normalizes (AHI < 5) in the non supine posture. A secondary aim was to determine if positional sleep apnea can be diagnosed accurately during a split-night study. Read more…
National Heart Lung and Blood Institute: What Is Sleep Apnea? Sleep apnea often goes undiagnosed. Doctors usually can’t detect the condition during routine office visits. Also, there are no blood tests for the condition. View an animation that shows how air flow to the lungs can be blocked, causing sleep apnea. Learn about the side effects of untreated sleep apnea. Read more…
JCSM: Clinical Guideline for the Evaluation, Management and Long-term Care of Obstructive Sleep Apnea in Adults. Guideline Objective: This guideline is designed to assist primary care providers as well ass sleep medicine specialists, surgeons, and dentists who care for patients with OSA by providing a comprehensive strategy for the evaluation, management and long-term care of adult patients with OSA. Read more…
The 2009 AASM guidelines relating to the treatment of positional therapy state:
“Positional therapy, consisting of a method that keeps the patient in a non-supine position, is an effective secondary therapy or can be a supplement to primary therapies for OSA in patients who have a low AHI in the non-supine versus that in the supine position (Guideline).21 Because not all patients normalize AHI when non-supine, correction of OSA by position should be documented with PSG before initiating this form of treatment as primary therapy (Consensus). A positioning device (e.g., alarm, pillow, backpack, tennis ball) should be used when initiating positional therapy (Consensus). To establish the efficacy of a positioning device in the home, providers should consider the use of an objective position monitor (Consensus). Treatment-specific outcome indicators to monitor with therapy include self-reported compliance, objective position monitoring, side effects, and symptom resolution (Consensus).”

